$SLS REGAL's flawed assumptions
SELL
Based on the most recent update from SELLAS Life Sciences regarding the Phase 3 REGAL trial, the study has made headlines for a "positive" delay: death events are accumulating significantly slower than statistical models predicted. As of late December 2025, the trial had recorded only 72 pooled events, missing the year-end target of 80 events required to trigger the final analysis. While bulls hope that this extended pooled survival is driven by the efficacy of the GPS arm, there is a distinct possibility that the trial's statistical assumptions were fundamentally flawed from the outset.
I belive the baseline survival of the control arm has been severely underestimated, hence "unexpected" longevity may simply reflect the natural history of the specific patient population enrolled rather than a drug effect. This potential miscalculation of baseline survival is not unique to REGAL but appears to be a systemic issue inherited from earlier studies of galinpepimut-S.
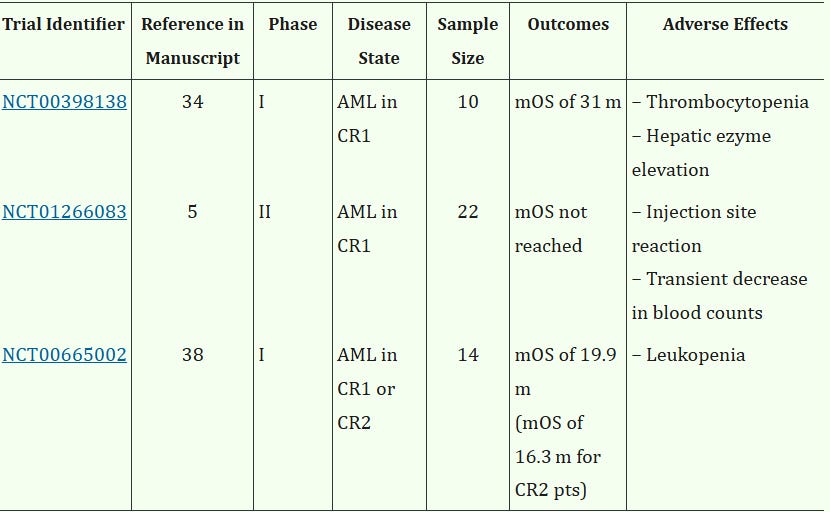
While historical Phase 1/2 trials of galinpepimut-S (GPS) report impressive median Overall Survival (mOS) figures that appear to outperform standard benchmarks for transplant-ineligible patients, these comparisons likely suffer from a critical selection bias regarding the fundamental definition of "ineligibility." In the broader relapsed AML population, the vast majority of patients deemed transplant-ineligible fall into this category due to poor physical condition, advanced age, or significant comorbidities, with only a minority (estimated at ~20%) excluded solely due to the lack of a compatible donor. However, the strict enrollment criteria of these past trials (mandating good performance status (ECOG), and okay-ish organ function) effectively filtered out the frail patients that dominate historical control datasets. Consequently, these earlier GPS cohorts were likely enriched for a specific, biologically distinct subset of patients: those who were physically fit enough for transplant but were ineligible purely due to donor unavailability. Since physical fitness is one of the strongest independent predictors of survival, comparing this "fit but unmatched" population against historical controls composed largely of "medically unfit" patients creates a baseline survival mismatch that may have artificially inflated the perceived efficacy of the investigational agent before the Phase 3 REGAL trial even began.
REGAL
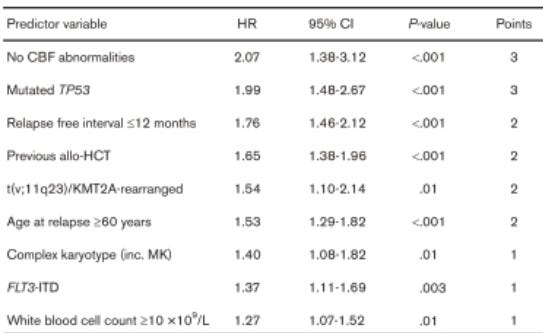
REGAL likely suffers the same selection bias as past GPS trials. This selection bias becomes evident when mapping the REGAL inclusion and exclusion criteria against established prognostic variables in AML (Table 1). First, the requirement for hematologic recovery (specifically an Absolute Neutrophil Count (ANC) >1,000/µL and Platelets >20,000/µL) effectively filters out patients with persistent marrow failure or aggressive, proliferative disease, factors which are strongly associated with poor outcomes.
Furthermore, the mandate that patients must have “recovered to Grade 0 or 1” from prior toxicities, possess adequate renal/hepatic function (excluding End Stage Renal Disease), and maintain an ECOG status of 0–3 systematically removes the frailest subset of the population—those with the “accumulated damage” that typically drives early mortality.
Critically, the requirement for a lymphocyte count >300/µL not only ensures vaccine mechanism but also serves as a proxy for immune competence, excluding those with profound immunosuppression who statistically fare worse.
Beyond these inclusion criteria, the composition of the Best Available Therapy (BAT) arm poses a specific statistical threat, particularly regarding the introduction of Venetoclax. Since Venetoclax only received FDA approval for AML in late 2018, the majority of patients enrolling in the REGAL trial (beginning in 2020) were likely “Venetoclax-naïve” at the time of study entry. This is a critical distinction: because the trial enriches for physically fit patients (ECOG 0–2), their first-line treatment was almost certainly intensive chemotherapy (standard “7+3” induction) rather than Venetoclax-based regimens, which are reserved for the unfit. Consequently, when these patients relapse and are randomized to the BAT arm, they are exposed to Venetoclax and HMA for the first time, a setting where drug-naïve patients demonstrate significantly superior outcomes compared to those with prior exposure.
While the REGAL trial design anchors its power calculations on a median Overall Survival (mOS) of just 8.0 months for the control group, real-world data suggests this baseline may be dangerously conservative. In r/r AML retrospective cohorts, patients achieving a composite Complete Remission (cCR) (which is CR2 for them) with HMA/Venetoclax demonstrated a staggering median OS of 21.6 months.
It is important to contextualize this figure: this 21.6-month benchmark is likely inflated by the inclusion of patients who successfully bridged to allogeneic transplant—a pathway closed to the REGAL “transplant-ineligible” population. However, even when discounting the transplant effect, the trial’s assumption that a modern, remission-selected control group will expire in just 8 months appears increasingly tenuous.
This pharmacologic advantage is compounded by a genetic selection bias. By selecting for “healthier” patients with robust hematologic recovery and slower disease kinetics, the trial likely inadvertently enriches the cohort with patients whose genetic mutations not just make them healthier but also Venetoclax super responders—specifically NPM1, IDH1/2, and TET2.
Crucially, this enrichment is reinforced by the subjective exclusion of any patient with an “estimated life expectancy <6 months” or “serious concurrent illness.” This criterion grants investigators the discretion to preemptively remove patients displaying the rapid clinical deterioration often driven by adverse mutations . By systematically censoring these “rapid progressors” before they can be randomized, the trial effectively amputates the left tail of the survival curve.
This leaves a sanitized control arm dominated by the “Venetoclax Super Responders” (NPM1, IDH) who not only have inherently slower-growing disease but also possess specific sensitivity to BCL-2 inhibition.
Evidence confirms that patients with NPM1 mutations, for instance, display exceptional sensitivity to BCL-2 inhibition, achieving response rates as high as 66%. Similarly, IDH1/2 mutations are highly predictive of deep, durable responses to Venetoclax-based salvage therapy. Conversely, the “poor responders” with FLT3-ITD or TP53 mutations are frequently filtered out by rapid disease progression during the induction window, effectively removing them from the “responder” dataset before they can impact the BAT statistics.
The trials Venetoclax-naïve population enriched for sensitive mutations could drive the control arm’s survival well beyond the 12-month mark, fundamentally undermining the trial’s statistical assumption of an 8.0-month baseline mortality.
Furthermore, the “Best Available Therapy” landscape has shifted during the trial’s lifespan. Most notably, the approval of revumenib in late 2024 provides a potent targeted option for patients with KMT2A mutations (roughly 5–10% of cases)—a subgroup previously associated with one of the poorest OS outcomes in AML.
Conclusion
In short, the recent “positive” news about the slow death rate in the REGAL trial is likely misleading. Bulls believe this means the GPS vaccine is working, but the evidence points to a different problem: the control group is simply living longer than the trial planned for. By strictly selecting for healthy patients and giving them powerful modern drugs like Venetoclax for the first time, the trial has created a control group of “Super Responders.” These patients are likely to survive much longer than the 8-month baseline the study used for its math.
As the control group’s survival stretches to 12 months or more, it becomes nearly impossible for the vaccine to prove it is statistically better, with the current implied pooled mOS.
Galinpepimut-S is fighting against a highly effective standard of care that it wasn’t designed to beat. Because there is a high chance the trial will fail to show a clear difference against this strong control group, I believe the current stock price is wrong. SELL
Sources
https://pmc.ncbi.nlm.nih.gov/articles/PMC3148903/
https://pmc.ncbi.nlm.nih.gov/articles/PMC4617516/
https://ashpublications.org/bloodadvances/article/9/2/425/535281/Things-like-AML-salvage-go-better-with-VEN-etoclax
https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2021.649209/full
https://pmc.ncbi.nlm.nih.gov/articles/PMC12329292/
https://pubmed.ncbi.nlm.nih.gov/40402082/
https://ascopubs.org/doi/10.1200/JCO.2023.41.16_suppl.e19007
https://pmc.ncbi.nlm.nih.gov/articles/PMC5364786/
https://pmc.ncbi.nlm.nih.gov/articles/PMC12056740/


First of all I have to say thank you for taking a scientific approach in analysing Sellas. I mean this is really good to see given that there is so much shouting around on this topic and it is bloody hard to have a deeper discussion. I have been digging through Sellas for a long time and want to point out following problems that I see in your analysis:
The "Futility" issue (IDMC meetings)
The first analytical problem to me is the August 2025 IDMC (and also previous) recommendation. If the BAT arm and the GPS arm were performing similarly (or worse), the Hazard Ratio would approach 1.0. In such a scenario, the IDMC—which sees unblinded data—would have likely halted the trial for futility during the August 2025 (or earlier) review. The IDMC recommended the trial continue without modification. This implies that even with the "slow event accrual," there is still a statistically significant separation between the two curves that justifies reaching the 80th event.
Misapplication of Venetoclax "Super Responder" Data
That 21.6-month figure almost always includes patients who bridge to a Stem Cell Transplant (SCT). In AML, transplant is the only "reset button" for survival, whereas the REGAL trial specifically enrolls patients who are not candidates for SCT. For relapsed/refractory (R/R) AML patients who achieve CR2 but do not go to transplant, the mOS for HMA/Venetoclax is historically closer to 6.5–9.0 months, not 21.6.
The "Event Velocity" vs. "Salvage" Logic
Slow death rates because of better salvage therapies like Revumenib - salvage therapy extends life after a relapse. However, to reach a pooled mOS of 13.5+ months (which SELLAS reported as a blinded aggregate in early 2025), the patients must stay in remission or stay alive longer initially.
• Immunotherapy Signature: In clinical trials, a "slow-down" or "plateau" in deaths late in a trial is a classic hallmark of immunotherapy (vaccines), where responders simply stop relapsing. Control arms (BAT), even with modern salvage, typically show a steady, predictable decay in survival.
• The Math: If only 1.0 death per month occurred in 2025, it suggests the remaining survivors are concentrated in one arm that has reached a survival plateau. If both arms were simply "living longer due to salvage," the event accrual would be slower but still steady, not a near-total halt.
The "Lymphocyte Count"
Requiring >300 lymphocytes/µL filters out the sickest patients, padding the BAT arm. While 100% true, it most definitely gives a boost to GPS, because this is a vaccine; it requires a functioning immune system to work. By filtering for immune-competent patients, the trial is also ensuring that the GPS arm is at its maximum potential efficacy. If the trial were "diluted" with immunosuppressed patients, the vaccine would fail regardless of how the BAT arm performed.
Genetic Enrichment (NPM1/IDH)
If the trial is enriched for NPM1 (intermediate risk), the BAT arm does better. But if the trial is enriched for the typical CR2 population (high-risk/WT1+), GPS has a biological "home field advantage." You assume the selection bias only helps the control, ignoring that these same "healthy" fit patients are exactly the ones most likely to mount the robust T-cell response GPS requires to succeed.
I mean I agree with you 100% that we will see a totally different BAT arm mOS in REGAL study. Given the differences in salvage therapies what have come to market after phase 2 study, I have no doubt that BAT arm will produce a mOS in the range of 14-18 months. My view simply is that GPS arm will benefit even more from those new salvage therapies and will get to 40+ months mOS. It is a actually a statistical task – if you run statistical models with hard anchor data (enrollment pace, interim deaths, etc.), then you see that in no way can BAT arm mOS be lower than 13-14 months and at the same time you also need plateauing in GPS arm to get to this very low number of deaths. But most importantly, IDMC who sees unblinded data, has absolutely no point to say “continue without modification”, if GPS and BAT are not separating.
So great write up there is hope for humanity. 10% of the population would be expected to be eligible for revuforj and half of them should transplant! My napkin math with all of this factored in gives this trial a 1-8 chance of hr < .64 (bar of success) if expected bat mos is 13m (could be higher). A similar phenomena sunk glycomemtics, with control arm having a mos >12 and they didn't have revuforj or the filtering. This screams fail. I have puts.